Cardiovascular diseases (CVDs) have become a major cause of death of women globally.(1) CVDs are diseases affecting the heart or blood vessels, including Coronary Heart Disease (CHD), stroke, congenital heart disease, peripheral arterial disease, rheumatic heart disease, and a pulmonary embolism.(2) In 2000, the number of female mortality due to CVDs was estimated to be around 7.2 million deaths, and it increased gradually to nearly 9 million deaths in 2016.(3) In Indonesia, the diseases have threatened Indonesian women’s health. Despite outdated, Indonesia Basic Health Research (Riskesdas), a national household health survey conducted every three years, in 2007 reported that IHD and stroke were the second and third cause of death in Indonesian women aged 45–54 years (11% and 9.1%, respectively), while stroke was the most leading cause of death in women in the age group 55–64 (20.7%) and over 65 (24.4%).(4) Thus, it is shown that CVDs have become crucial health issues in Indonesian women.
However, despite the significant figures of CVDs in Indonesian women, CVDs continue to be sidelined in Indonesian women health development agenda. Why have CVDs in Indonesian women been neglected? One of the influencing factors of the negligence of CVDs in women is gender, a socially constructed characteristics given to male and female.(5) Gender influences the priority of women’s health agenda, risks of CVDs, social determinants of the diseases and treatment of CVDs.
Women’s health priority
Gender roles shape the priority of women health development. Gender roles are socially constructed roles applied to men and women, which determine what is acceptable for them in social life.(6) Since pregnancy and childbirth are considered as women’s roles, health services provided for women mostly focus on women’s reproductive capacity.(7) Therefore, health services related to maternal health have become a priority of women’s health in Indonesia, even though health problems experienced by women tend to be beyond maternal health.
Man’s disease
It is argued that CVDs are the priority of men’s health as they are considered as men’s diseases.(8) However, Indonesian women are more likely to experience the diseases. According to Riskesdas in 2013, the prevalence of stroke in the age group ≥ 15 was slightly higher in women (12.1 ‰) than men (12 ‰) in 2013.(9) Similarly, CHD prevalence in women was (1.6%) slightly higher compared with men (1.3%) both in 2013 and 2018.(9,10)
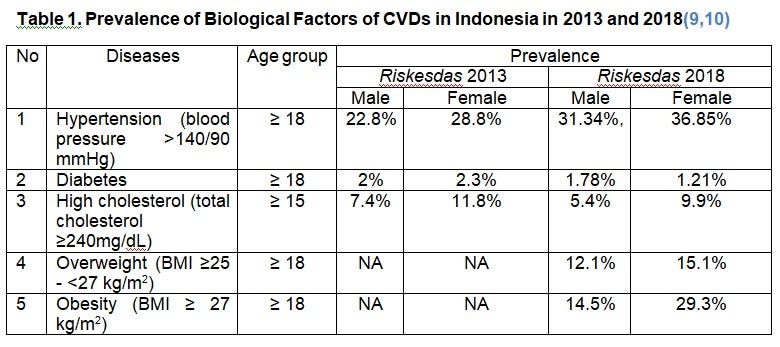
Furthermore, Indonesian women appear to be more prone to some risk factors of CVDs. According to World Health Organization, CVDs are caused by biological and behavioural risk factors.(2) Biological factors, namely hypertension, diabetes, high cholesterol, overweight and obesity, can inflame blood vessels, which could block blood circulation through the heart and brain. According to Table 1, Indonesian women appear to have a higher risk of CVDs compared with men since they are more likely to experience the biological factors of the diseases.

Meanwhile, behavioural risk factors of CVDs, which are an unhealthy lifestyle, tobacco use and alcohol consumption,(2) are less likely to become risk factors of CVDs in women. This is because smoking and alcohol consumption prevalence in any age groups were lower in women than men.(11) Moreover, although poor physical activity is also one of the factors of CVDs, there seems to be a lack of study examining this factor in Indonesia.(12)
To sum up, the figures above indicate that CVDs are not only men’s business, but they are also women’s health issue. This is because women are more likely to experience CVDs and some risk factors of the diseases. Therefore, it is crucial to address CVDs in Indonesian women.
Social determinants of CVDs
Gender interweaves with the social determinants of CVDs in women, namely socioeconomic status and education. Alessie et al. discover that women in poor socioeconomic status are more likely to experience CVDs.(13) This is because, first, impoverishment exacerbates women’s access to education.(14) Indonesian women, both in a rural and urban area, were less literate compared with men and living in adverse economic condition widened the literacy gap between men and women.(15) Women in socioeconomic quintile 5 had slightly lower literacy rate than men (98.18% and 99.24%). Meanwhile, in quintile 1 group, women’s literacy rate was lower by 6.21% compared with men.(15) Due to the limitation of financial resources, men’s education tends to be more prioritized than women’s education. This could be because women are expected to play their roles as caregivers rather than attending school. However, having higher education is associated with a lower risk of CVDs.(16) Having adequate educational attainment could lead to excellent knowledge about a healthy lifestyle and functional health literacy which could be protective factors of CVDs. Therefore, due to poor socioeconomic status and education, women are more likely to have a higher risk of CVDs.
Second, low socioeconomic status increases the barrier for people to access health services.(17) In Indonesia, women tend to be economically inferior as they are less likely to participate in labour, and when they work, they tend to receive a lower payment than men.(15) The lower employment and pay rate of women are influenced by gender. At the individual level, gender inequality in education contributes to the low payment rate of women. As women have a lower education level than men, they are more likely to work in informal sectors, such as street vendors or petty traders, which have lower wages. Gender roles and responsibilities are also associated with the lack of women’s participation in labour. For instance, since domestic work is considered as women’s roles and responsibilities, women tend to stay at house rather than working, or they are more likely to have informal jobs which enable them to do household chores due to flexible working hour.

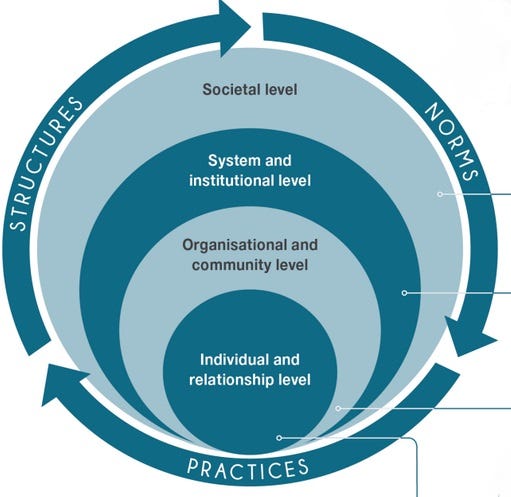
Furthermore, at the relationship level, the weak support from husband or family could hinder women from getting a job. For example, men tend not to support their wives to work since they consider themselves as the breadwinner. Meanwhile, at an organizational level, gender roles influence organization regulation on recruitment which affects women’s participation in labour. For instance, some work is restricted for men, and this prevents the organization to recruit women.(18) Moreover, at a system or an institutional level, having gender-sensitive policies on the gender composition of the workforce could promote equal working opportunities for both men and women. However, the unavailability of specific Indonesia’s law mentioning gender quota at the organization level, except in parliaments, tends not to support women’s participation in labour. Therefore, being unemployed or having little money could lead to an economic imbalance between men and women, which forces women to be financially dependent on men. This could exacerbate women’s risk of CVDs because if women have little control over financial resources, it could be difficult for them to access health services related to CVDs.
Health treatments for CVDs
It is assumed that findings of medical research related to Non-Communicable Diseases (NCDs), including CVDs, are applicable for both men and women, although most of the research recruit male as their respondents.(19) However, recent findings discover that sex differences exist in CVDs, particularly in the symptoms of CVDs. The symptoms of CVDs tend to be less symptomatic in women compared with men, and this prevents early diagnoses of CVDs in women.(20) Due to different manifestation, women receive different treatment than men with similar symptoms; for example, women are asked fewer questions and are received fewer treatments and diagnostic tests.(21) Thus, gender and sex differences should be taken into consideration in conducting medical research related to CVDs and providing health treatment for women.
Current national health program for CVDs
Responding to the growing burden of CVDs, The Government of Indonesia (GoI) has established Posbindu to overcome NCDs, including CVDs since 2012.(22) Posbindu is a community-based intervention which aims to provide early detection services and monitor risk factors of NCDs for people aged 15 and above.(22) According to the Indonesia Ministry of Health in 2018, the proportion of village conducting Posbindu (43.9%) in 2018 met the Indonesia Ministry of Health target (40%).(23)
However, there were gaps in the distribution and implementation of the service. First, provinces which had a high percentage of villages conducting Posbindu were mostly in the western part of Indonesia, where the capital city of Indonesia is located. Meanwhile, provinces in the eastern part of Indonesia were less likely to have Posbindu, for example, the proportion of village conducting Posbindu in Papua and West Papua was under 8%.(23) Therefore, equal distribution of this program should be improved. Second, some studies highlight some improvements which are needed for the Posbindu implementation. For instance, Putri and Andriyani conducted a study on 38 Posbindu for elderly in Bandung, West Java Province.(24) They found that the Posbindu had lack of health assessment tools, and some community health volunteers did not have knowledge and skills in operating the equipment for health assessment. Therefore, this could limit early detection services delivered in Posbindu.
Conclusion and recommendation
In conclusion, due to gender bias, CVDs have not become the priority of Indonesian of women’s health and the diseases are considered as men’s diseases. It also could lead to higher risks of CVDs and unequal treatment of CVDs for women. The fact that CVDs are not only men’s health problem and the diseases are significant health burden for Indonesian women suggest that the focus of Indonesian women health should be redefined by incorporating CVDs into Indonesian women health development agenda. It is also crucial to address the gender context of CVDs to overcome the exacerbation of women’s vulnerability to the diseases. Furthermore, although the GoI has implemented Posbindu to address CVDs in women, some improvements are needed in the implementation of the program.
As a recommendation, there is a need to strengthen research and the existing health program for CVDs in women. First, updated data of the causes of women death is urgently needed since, as mentioned above, the latest data of the causes of women death was provided by Riskesdas in 2007. Second, conducting research about physical health in men and women and the relation between physical health and CVDs in Indonesia also should be done. Third, more research about CVDs with a gender approach should be conducted, particularly research about CVDs treatment, to have a better understanding of the gender differences in CVDs in Indonesia and support the government in providing suitable intervention for women. Furthermore, improving the distribution, facilities and human resources of Posbindu should be conducted to enhance the quality of Posbindu services. More research and reports about the existing program are also needed to improve the program’s monitoring and evaluation.
References
1. World Health Organization. Non-Communicable Diseases: A Priority for Women’s Health and Development [Internet]. World Health Organization; 2010 [cited 2019 Oct 15]. Available from: https://www.who.int/pmnch/topics/maternal/2011_women_ncd_report.pdf.pdf
2. World Health Organization. Cardiovascular diseases (CVDs) [Internet]. World Health Organization. 2017 [cited 2019 Oct 24]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
3. World Health Organization. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region 2000–2016 [Internet]. World Health Organization (WHO); 2018 [cited 2019 Oct 23]. Available from: https://www.who.int/healthinfo/global_burden_disease/GHE2016_Deaths_WBInc_2000_2016.xls
4. Indonesia Ministry of Health. Basic Health Research (Riskesdas) 2007 [Internet]. Indonesia Ministry of Health; 2007 [cited 2019 Oct 10]. Available from: http://labdata.litbang.depkes.go.id/images/download/laporan/RKD/2007/lap_rkd07.pdf
5. World Health Organization. What do we mean by sex and gender? [Internet]. 2013 [cited 2019 Dec 17]. Available from: http://www.who.int/gender/whatisgender/en/
6. Gelb K, Pederson A, Greaves L. How have health promotion frameworks considered gender? Health Promotion International. 2012 Dec;27(4):445–52.
7. Bustreo F, Knaul FM, Bhadelia A, Beard J, Araujo de Carvalho I. Women’s health beyond reproduction: meeting the challenges. Bull World Health Organ. 2012 Jul 1;90(7):478–478A.
8. Bots SH, Peters SAE, Woodward M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. BMJ Glob Health. 2017 Mar;2(2):e000298.
9. Indonesia Ministry of Health. Basic Health Research (Riskesdas) 2013 [Internet]. Indonesia Ministry of Health; 2013 [cited 2019 Oct 10]. Available from: http://labmandat.litbang.depkes.go.id/images/download/laporan/RKD/2013/Laporan_riskesdas_2013_final.pdf
10. Indonesia Ministry of Health. Basic Health Research (Riskesdas) 2018 [Internet]. Indonesia Ministry of Health; 2018 [cited 2019 Oct 10]. Available from: http://labmandat.litbang.depkes.go.id/images/download/laporan/RKD/2018/Laporan_Nasional_RKD2018_FINAL.pdf
11. Mboi N, Murty Surbakti I, Trihandini I, Elyazar I, Houston Smith K, Bahjuri Ali P, et al. On the road to universal health care in Indonesia, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2018 Aug;392(10147):581–91.
12. Schroders J, Wall S, Hakimi M, Dewi FST, Weinehall L, Nichter M, et al. How is Indonesia coping with its epidemic of chronic noncommunicable diseases? A systematic review with meta-analysis. PLOS ONE. 2017 Jun 20;12(6).
13. Alessie RJM, Angelini V, van den Berg GJ, Mierau JO, Viluma L. Economic conditions at birth and cardiovascular disease risk in adulthood: Evidence from post-1950 cohorts. Social Science & Medicine. 2019 Mar 1;224:77–84.
14. Yang J, Huang X, Liu X. An analysis of education inequality in China. International Journal of Educational Development. 2014 Jul;37:2–10.
15. Indonesia Ministry of Women’s Empowerment and Child Protection. Indonesian Women Profile 2018 [Internet]. Indonesia Ministry of Women’s Empowerment and Child Protection; 2018 [cited 2019 Oct 17]. Available from: https://www.kemenpppa.go.id/lib/uploads/list/d9495-buku-ppi-2018.pdf
16. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic Status and Cardiovascular Outcomes. Circulation [Internet]. 2018 May [cited 2019 Nov 6]; Available from: https://www-ahajournals-org.ezp.lib.unimelb.edu.au/doi/abs/10.1161/CIRCULATIONAHA.117.029652
17. Tang KL, Pilote L, Behlouli H, Godley J, Ghali WA, for the GENESIS-PRAXY investigators. An exploration of the subjective social status construct in patients with acute coronary syndrome. BMC Cardiovascular Disorders. 2018 Feb 6;18(1):22.
18. Gorman EH, Mosseri S. How organizational characteristics shape gender difference and inequality at work. Sociology Compass. 2019;13(3):e12660.
19. Peters SAE, Woodward M, Jha V, Kennedy S, Norton R. Women’s health: a new global agenda. BMJ Global Health. 2016;8.
20. DeVon HA, Ryan CJ, Ochs AL, Shapiro M. Symptoms across the continuum of acute coronary syndromes: differences between women and men. Am J Crit Care. 2008 Jan;17(1):14–24; quiz 25.
21. Bonita R, Beaglehole R. Women and NCDs: Overcoming the neglect. Global Health Action. 2014;(0):1.
22. Indonesia Ministry of Health. Technical Guidlines for Posbindu PTM [Internet]. Indonesia Ministry of Health; 2012 [cited 2019 Oct 19]. Available from: http://p2ptm.kemkes.go.id/uploads/2016/10/Petunjuk-Teknis-Pos-Pembinaan-Terpadu-Penyakit-Tidak-Menular-POSBINDU-PTM.pdf
23. Indonesia Ministry of Health. Non-Communicable Diseases. In: Indonesia Health Profile 2018 [Internet]. Jakarta: Indonesia Ministry of Health; 2018. p. 247. Available from: http://www.depkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Data-dan-Informasi_Profil-Kesehatan-Indonesia-2018.pdf
24. Putri ST, Andriyani S. Needs and Problems of Posbindu Program: Community Health Volunteers Perspective. IOP Conf Ser: Mater Sci Eng. 2018 Jan;288:012139.
Penulis: Alya Hazfiarini
Editor: Ilham Akhsanu Ridlo